avril 23, 2024
Actu
Culture
Divertissement
Emploi
Environnement
Société
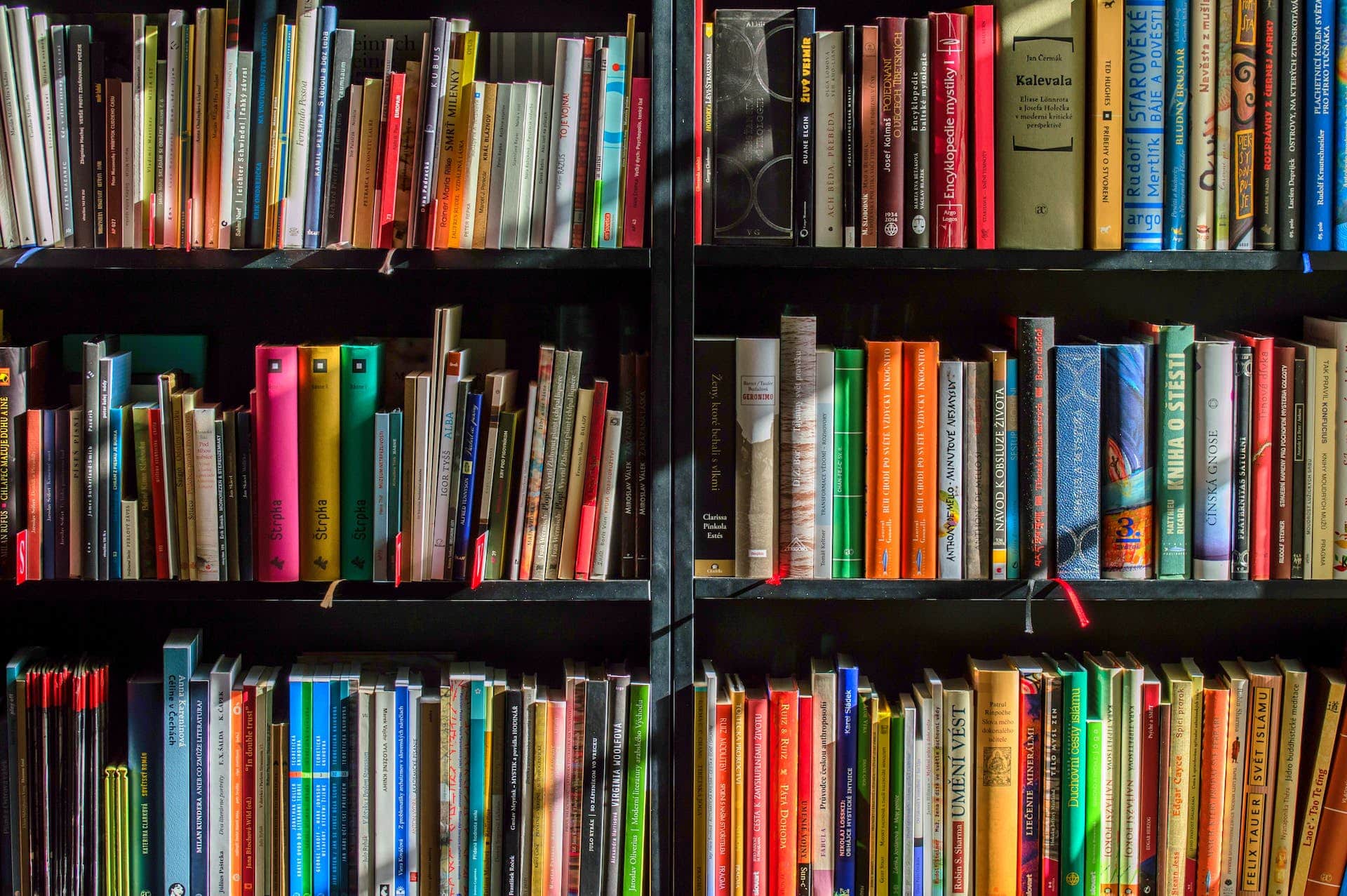
Comment les bibliothèques peuvent-elles s’adapter pour devenir des centres communautaires polyvalents ?
Aujourd’hui, nous allons aborder un sujet qui concerne un lieu que vous avez certainement fréquenté au moins une fois dans votre vie : la bibliothèque....
décembre 30, 2023
Copyright 2024. Tous Droits Réservés